Emergency Services Shows Courage in the Face of COVID-19

You cannot communicate too much in a crisis. --Scott Reeves, MD
COVID-19 has consumed the headlines for months now, to the point where most of us have grown weary of the topic. But as healthcare providers, we don’t have the luxury of giving in to that fatigue. Too many lives depend on us.
Emergency Services staff in the Burnet and Liberty Campus EDs know this all too well. They are the frontline of the frontline. And they have shown exceptional courage and dedication to their work throughout this pandemic.
“We’re the front door of the organization in many ways,” explained Tonya Ross, RN, clinical director of the Burnet Campus ED and Urgent Care. “We tend to be disaster planners, and so we look for trends and patterns in the cases we see. We have a heightened sense of awareness because we are protectors of the organization. There’s a feeling that if we don’t pick up quickly enough on something at the front door, then what are we letting into our house?”
When COVID-19 began to surface in Wuhan and spread to Italy, Emergency Services staff was paying attention and thinking about what a surge plan might look like. They consulted with Nathan Timm, MD, Emergency Medicine, who directs the Office of Emergency Management, and Amber Antoni, RN, program manager, Emergency Management.
“Having that built-in connection with Nathan made it easier to weigh in on the conversations regarding the organization’s response and to vet some decisions around screening and testing, especially since 50 percent of our patients come into the hospital through the ED,” said Stephen Porter, MD, director, Emergency Medicine.
Based on annual simulations to test their business continuity plan, ED staff knew what questions to ask—How will we discharge inpatients to make room for new ones? Do we have enough personal protective equipment (PPE)? Do we have the right PPE? Do we need to set up a tent for testing or care outside the ED walls?
“Uncertainty was the overriding word,” said Scott Reeves, MD, senior clinical director of the Burnet and Liberty EDs. “When we realized COVID-19 was going to be a pandemic and that every healthcare entity in the U.S. would have to confront it, we changed our entire way of doing business. All we thought about for weeks was how to maintain our essential services while adapting to all the changes COVID-19 would bring.”
What those changes might be wasn’t exactly clear. Little was known about the disease. “When you go into emergency medicine, you understand you don’t have a choice about what you’re going to deal with every day,” said Reeves. “We did realize that COVID-19 would likely be more of a risk for adults than children, so it magnified the fear and anxiety that staff would be more vulnerable.”
Adding to that anxiety was the conflicting information coming from the Centers for Disease Control (CDC), the World Health Organization (WHO), local health departments and specialty organizations. The rapid changes in recommended protocols that sometimes occurred from one day to the next was confusing and a little unnerving.
Communication to the Forefront
To get ahead of the challenge, the Emergency Services leadership team ramped up from biweekly to daily phone calls. They participated on the hospital-wide COVID-19 Steering Committee and held town halls with staff twice a day for morning and evening shifts. They also sent out daily emails to their teams, referring them to the "Minutes with Michael" videos in CenterNews and the COVID-19 site on CenterLink.
“With so many unknowns and new information coming out every day, we quickly realized communication would be key,” said Laurie Gregor, RN, clinical director of the Liberty Campus ED. “It was important to have one source of truth so we could get everyone on the same page and moving in the same direction—especially since the truth was anything but static.”

In the ED, there's a heightened awareness, a sense of being protectors against what comes into the organization. -- Tonya Ross, RN
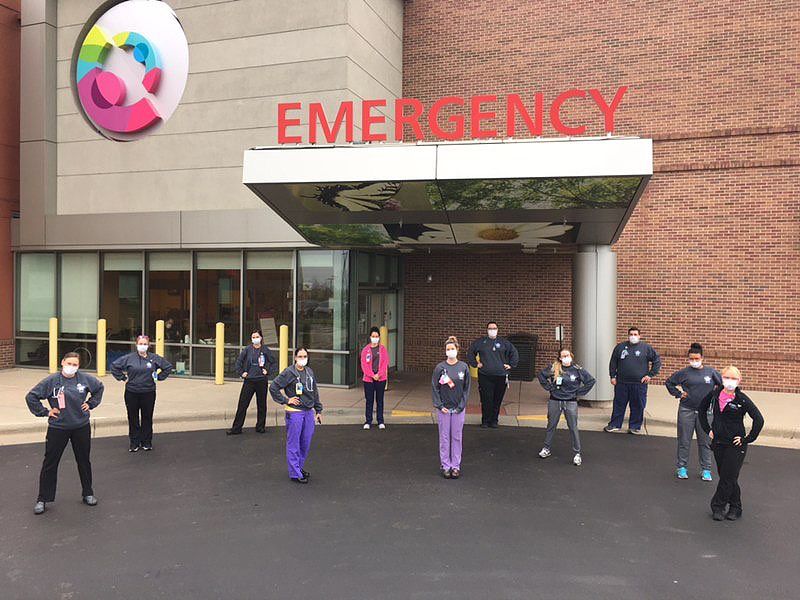
Liberty Campus ED staff, masked and ready to care for patients.
Not What We Expected
As a specialized area, the Emergency Services team recognized early on that it was important to keep staff healthy. "We blew up our schedules and developed a core team to provide care, then put together two other teams that rotated in and out for two-week intervals,” explained Gregor. “We kept the A and B teams separate, with the goal of reducing their exposure.”
They also assisted Safety Officer Jeff Simmons, MD, and Infection Control with developing testing algorithms for patients and staff. It was a heavy lift, but they accomplished it in a relatively short span of time.
Then in mid-March, it happened—or didn’t happen—depending on your point of view.
“In just over a week’s time, we saw the number of ED patients drop to about 35 to 40 percent of our usual volume” said Porter. “It was eerie. And it stayed like that through April, which is normally a busy time for us. Meanwhile, on the news, we were seeing images of healthcare providers in other cities wearing Hazmat suits and patients being intubated in hallways. The EDs had been turned into Intensive Care Units. It looked like a war zone. The quieter it was here, the more time we had to worry about the true risk we were facing.”
There was fear of catching the virus and bringing it home to family members. There was stress about how to juggle work schedules with childcare and homeschooling requirements. And there was great concern about the impact of delayed care for kids who weren’t being seen because of the pandemic.
Said Ross, “The emotion around all this has been intense. Some of our staff have serious underlying conditions, or they have family members who are vulnerable. But people still showed up. And they have been flexible and very supportive of one another. They want to be there and do what they are called to do. I am so proud of our team.”
Both EDs have an embedded liaison with the Employee Assistance Program to help staff who need a listening ear. Employee Health and Pastoral Care have also been available through Zoom meetings to offer support. At the Liberty ED, Gregor and her team started a Giving Grace program. Thirty people volunteered to be grace givers who encourage staff by sending notecards to coworkers or giving candy. At Burnet Campus, the approach was less formal. They created space where staff could step away for a moment or vent with a colleague. The primary goal was to build resilience
Key Takeaways
Despite its challenges, COVID-19 has been a rallying point for Emergency Services and Cincinnati Children’s as a whole. It’s also been a revelation.
“My biggest lesson is that you cannot communicate too much in a crisis,” said Reeves. “People are thirsty for information. There’s still a lot we don’t know about the disease, so we have to be comfortable saying we don’t have the answer, but we’re going to make every effort to get it. And then we have to make sure we are all saying the same thing, because it can really undermine staff confidence if you get different answers to the same question from different people.”
Said Gregor, “This has been the toughest time for me as a leader since I started working here in 1990, but I wouldn’t trade it for anything because I’ve learned a lot, including how important it is to have a presence and be face-to-face with your team. It’s been amazing to see everybody coming together for a common purpose—despite what they’re dealing with personally—to reassure families and be that solid care provider who gives great customer service even with all these changes going on in the background.”
“COVID-19 has been one big Safer Together moment,” said Ross. “We’re all here to advocate for each other’s safety, no matter what that is. I see our vision and mission amplified in everything and our leadership growing in the same direction. I hope we can sustain that momentum when things settle down and other priorities start to compete for our attention. It sounds trite, but our one-ness, our unity has been the best thing to come out of our COVID-19 work. We are a team, and we really are better together.”

Despite their own fear, our staff have continued to provide great care that is reassuring to families. --Laurie Gregor, RN
On a Personal Note...
“There is something really special about someone who chooses to work in the ED environment and thrives in it,” said Stephen Porter, MD, director of Emergency Medicine. “It takes a combination of real skills, confidence and the ability to connect with and offer compassion to people you’ve just met who are dealing with situations that range in seriousness from a stubbed toe to a life-threatening trauma or illness.”
Tonya Ross, RN, clinical director of the Burnet Campus ED and Urgent Care, agrees and shares the following thoughts about the ED staff and the “gifts” of COVID-19:
When I became a leader in the ED, I wanted to care for my team, and I said this aloud to the trauma nurses in my first meeting as director. No one spoke, but there was a palpable response in the room, a jolt that went through them. I struggled with their response for about a year afterward. What was it about the word ‘care’ that was such a trigger?
Then I remembered my own experience as a trauma nurse. In our day-to-day routine, you see the worst of the worst—to the point where you have to put on a little bit of armor before you come into work, and you can’t afford to let it down or you wouldn’t be able to do your job.
My staff are phenomenal. They know how to support each other in ways that feel authentic. They care about the patients they see and the ones they don’t see. And when our volumes dropped, they were, in a sense, laid bare because they were here, ready to do what we do best, but there was nobody to serve.
These are unusual times. I’m hearing people say they are tired in such a profound way that I’ve not heard before. But I remember our COO Steve Davis saying early on, “Look for growth in the trauma.”
I think Cincinnati Children’s response to COVID-19 has been so strong, it laid the foundation to begin to tackle issues (e.g., racial injustice) that have needed to be tackled for a long time. I am amazed and proud of the way we’ve spent time talking about these matters as an organization. In my 32 years here, I don’t remember that happening. Perhaps it’s because we are a little more vulnerable than in the past. But I also think we’ve made such great strides as one Cincinnati Children’s and in building a safe place, that an increasing number of us are ready to be the change that’s so desperately needed.
